Page 34 - Demo
P. 34
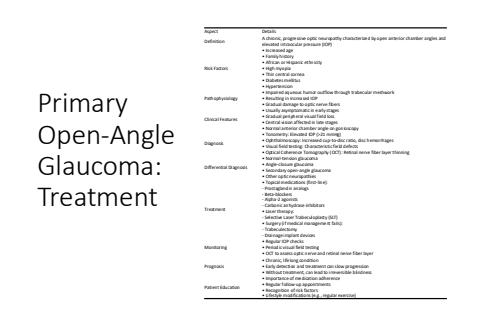
Primary Open-Angle Glaucoma: TreatmentAspect DetailsDefinition A chronic, progressive optic neuropathy characterized by open anterior chamber angles and elevated intraocular pressure (IOP)Risk Factors%u2022 Increased age%u2022 Family history%u2022 African or Hispanic ethnicity%u2022 High myopia%u2022 Thin central cornea%u2022 Diabetes mellitus%u2022 HypertensionPathophysiology%u2022 Impaired aqueous humor outflow through trabecular meshwork%u2022 Resulting in increased IOP%u2022 Gradual damage to optic nerve fibersClinical Features%u2022 Usually asymptomatic in early stages%u2022 Gradual peripheral visual field loss%u2022 Central vision affected in late stages%u2022 Normal anterior chamber angle on gonioscopyDiagnosis%u2022 Tonometry: Elevated IOP (>21 mmHg)%u2022 Ophthalmoscopy: Increased cup-to-disc ratio, disc hemorrhages%u2022 Visual field testing: Characteristic field defects%u2022 Optical Coherence Tomography (OCT): Retinal nerve fiber layer thinningDifferential Diagnosis%u2022 Normal-tension glaucoma%u2022 Angle-closure glaucoma%u2022 Secondary open-angle glaucoma%u2022 Other optic neuropathiesTreatment%u2022 Topical medications (first-line):- Prostaglandin analogs- Beta-blockers- Alpha-2 agonists- Carbonic anhydrase inhibitors%u2022 Laser therapy:- Selective Laser Trabeculoplasty (SLT)%u2022 Surgery (if medical management fails):- Trabeculectomy- Drainage implant devicesMonitoring%u2022 Regular IOP checks%u2022 Periodic visual field testing%u2022 OCT to assess optic nerve and retinal nerve fiber layerPrognosis%u2022 Chronic, lifelong condition%u2022 Early detection and treatment can slow progression%u2022 Without treatment, can lead to irreversible blindnessPatient Education%u2022 Importance of medication adherence%u2022 Regular follow-up appointments%u2022 Recognition of risk factors%u2022 Lifestyle modifications (e.g., regular exercise)